Identifying ‘step-down’ bed needs to improve ICU capacity and costs

- Industry
- Healthcare
- Location
- Ontario, Canada
- Goals
- Evaluate the needs of step-down beds to maximize ICU patient throughput, deliver efficiency and minimize cost
Achievements with Simul8
-
-
Projected $10 million of potential cost savings over span of 8 years
-
-
Identified average bed utilization rates based on multiple scenarios
-
-
Established evidence in reducing length of stay by up to 100 hours per patient
-
-
Gathered detailed evidence to reinforce decision-making using simulation
About the project
London Health Sciences Centre and Ivey Business School utilized Simul8 healthcare simulation software to evaluate the implementation of ‘step-down’ or 'level 2' beds, identifying positive impacts on ICU patient throughput, length of stay and costs.
In congested hospitals it can be common for patients to overstay at Intensive Care Units (ICU) due to blockages and imbalances in capacity. There are various reasons why an unnecessary stay in the ICU can be costly for hospitals:
- Clinically - patients occupy a service they no longer need
- Operationally - it disrupts flow from upstream units
- Financially - ICU beds are more expensive than ward beds
To meet this challenge, step-down beds (also known as level 2 beds) are an increasingly popular and less expensive alternative to ICU beds.
London Health Sciences Centre (LHSC), one of Canada’s largest acute-care teaching hospitals, together with the team at Ivey Business School for Health Innovation, utilized simulation to identify the impact of using step-down beds in the University Hospital’s Medical Surgical Intensive Care Unit (MSICU).
Analyzing historic data, it was identified that of patients treated in the ICU in 2014, 660 out of 864 were recorded with a NEM score (a measure of nursing workload requirements) that would have enabled those patients to eventually step down into a level 2 ward - saving valuable potential resources. The key goal of LHSC’s research was to evaluate if additional ICU bed capacity could be released through the use of level 2 beds and how many beds would be needed to deliver efficiency and cost savings.
The team also wanted to assess whether NEM scoring could be used to identify when a patient could be stepped-down and help estimate level 2 bed needs. Using Simul8, the team could consider a wide range of parameters to fully assess the impact on patient flow, length of stay, utilization and costs - all within a safe, risk-free environment.


"With many complex processes and parameters involved, we needed simulation to be able to test the implementation of step-down beds to meet our objectives of maximizing patient throughput, while minimizing the length of stay in the ICU and cost to the hospital."
Ivey International Centre for Health Innovation

Taking every factor into consideration using simulation
When looking at bed needs, every process and decision within a hospital can impact capacity and patient flow. With a huge range of parameters to consider, planning any changes to the process cannot be achieved in silo. How can you be confident that changes won't have ramifications elsewhere?
This is a key reason why LHSC utilized Simul8 healthcare simulation software over other analytical methods. Using Simul8, the team could take a diverse range of factors into consideration to ensure accurate results, including:
- Arrival rates - these vary throughout the hour of the day, day of the week, as well as seasonally.
- Bounce backs - patient flow isn’t always linear, a patients’ journey can take them through various departments, such as the ICU and operating rooms.
- Patient’s health and death probability change over time - for example, the odds of a patient’s survival increase as they spend more time in the ICU.
- Off-service patients and length of stay - the misplacement of patients into wards that they are not originally supposed to go can lead to an increase in length of stay and costs.
- NEM scoring process - the level of nursing care where a patient could be considered for the step-down and how this score changes over time.
Key project steps
Utilizing existing data to create step-down rules
The team were able to utilize existing data from LHSC’s patient management system, containing patient arrival times and characteristics, as well as precise patient transfer files.
This provided a view of the individual beds where the patients came to and from in each hospital unit. Additionally, as nursing workloads are recorded at upon arrival and once daily, as well as when the patient leaves the unit, the team had access to data on the NEM scoring process for every patient that went into the MSICU.
Distributions could then be created, along with a patient flow matrix and step-down rules to power the simulation.
Planning the simulation
To take into account the various entry points and congestion that occurs in the hospital, and assess how these complexities could potentially impact the use of level 2 beds, the team made the decision to simulate the entirety of the hospital patient flow.
The simulation also included stochastic attributes, such as the probability of death, to give a fully accurate representation of what really happens in the ICU.
Validation and testing step-down bed scenarios
After validating the accuracy of the base simulation against the current system performance, the team could run different scenarios to identify the best approach to the implementation of level 2 beds:
Scenario oneAdding up to 20 beds in a new level 2/step-down unit, with no changes to existing MSICU beds.
Scenario twoRe-allocation of existing capacity by converting some of the 25 MSICU beds into level 2 beds.
Scenario threeAdding 5 extra beds to bring total MSICU capacity to 30 beds, allocating these between the MSICU and a new level 2 unit.


"The results from the simulation were very helpful and provided additional evidence to reinforce our decision-making. It has been a very useful project to be involved with on a very relevant question."
London Health Sciences Centre
Project Results
$10 million of potential cost savings
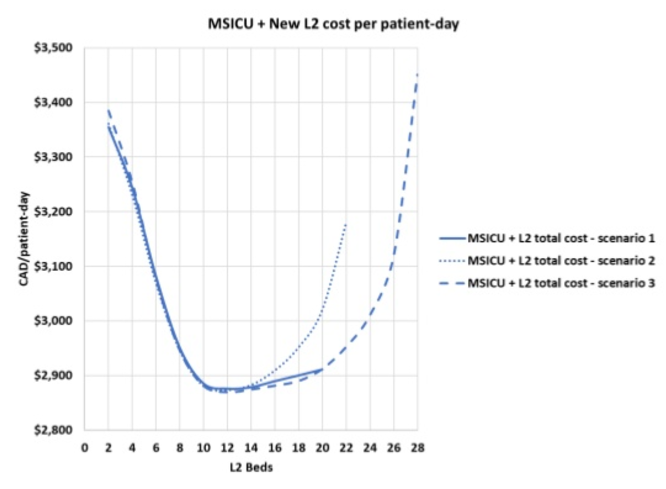
A key driver for the project was to evaluate potential cost savings of using level 2 beds. Using the simulation results, the estimated short-term and long-term costs of each scenario could be compared.
The simulation results showed that as more level 2 beds were added, costs start to drop dramatically to as much as $600 per patient/day - reaching a minimum cost at around 12 beds across all scenarios due to economies of scale.
When more than 12 beds are added, there is an increase in idle capacity and costs start to increase as the MSICU is further reduced in size. This showed that the optimum threshold would be between 10 to 14 level 2 beds.
As the simulation could run years into the future, LHSC could see the longer-term cost savings of implementing each of the scenarios – with potential savings of almost $10 million dollars over the span of eight years, compared to the baseline simulation.
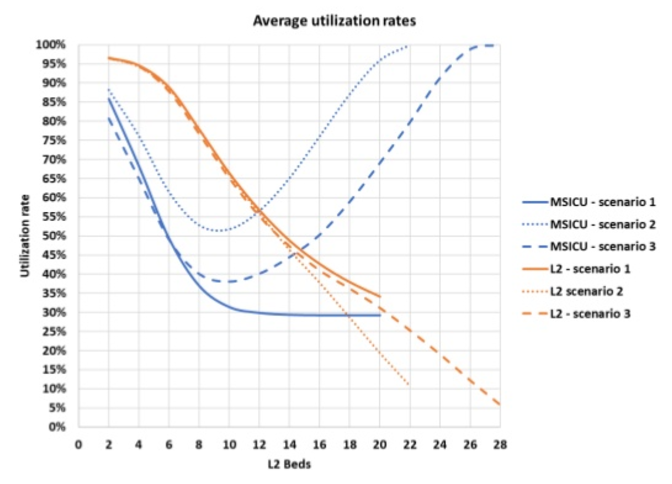
Utilization rates for each scenario
Although empty beds are essential to have in an ICU for surges in patient arrivals, they must be balanced against having excess idle capacity that wastes resource and costs.
The simulation results showed that in scenario one, where a completely new unit is added, level 2 bed utilization rates drop dramatically and keeps falling up to 30%, meaning there would be too many beds not in use for this to be a viable option.
Scenario two proved to strike an ideal balance, using between 8 to 10 level 2 beds from existing capacity provided better utilization, with the ability to accommodate surges in patients throughout the year.
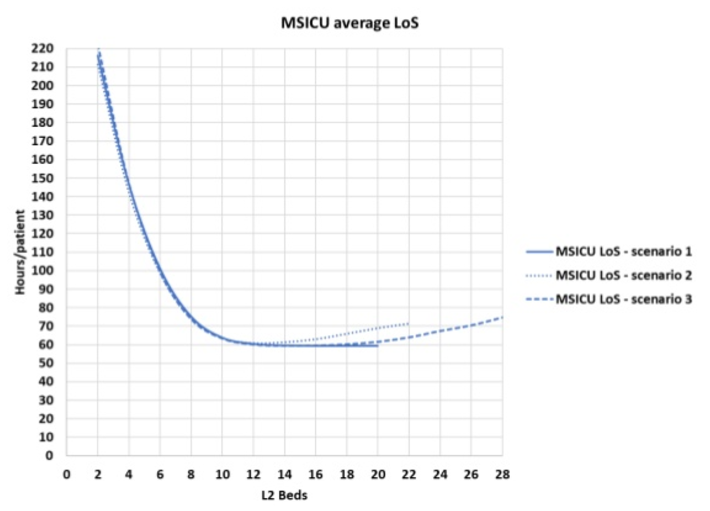
Reducing MSICU length of stay
The simulation showed that as the number of level 2 beds increased, patient length of stay could also drop dramatically.
From the baseline of 160 hours per patient, in the beginning there is a sharp increase. As patient flow into the level 2 unit improves, there would be a sharp drop – eventually reaching a threshold of roughly 60 hours. In the scenarios where beds are reallocated from existing capacity, the level 2 unit would eventually become bottlenecked by the MSICU, with length of stay starting to increase again from this point.
Reducing patient length of stay by up to 100 hours per patient would provide substantial extra capacity as ICU beds are released to receive new patients that emerge from the operating room.
Achievements with Simul8
Using Simul8, LHSC could quickly run each of the scenarios and get detailed results around the key metrics of cost, length of stay and utilization of the MSICU and level 2 beds.
Across all scenarios, it was found that simulating level 2 beds into the current patient flow generally provided a positive impact - reducing occupancy, decreasing length of stay of MSICU patients, as well as saving and costs. Comparing the three different scenarios to the baseline results, it was found that converting existing capacity from the MSICU would provide an optimal balance on return, rather than adding new, additional capacity.
Adding the NEM scoring process and the stochastic death probability process into the simulation proved to also be very useful, helping identify the point where patients could be stepped down from an ICU bed to a level 2 bed. With the project delivering many valuable insights, LHSC are now looking at using simulation in their sister hospital, Victoria Hospital, as well as creating simulations to look at the impact of having dedicated long-stay beds.
Webinar
Discover how simulation was used to evaluate ‘step-down’ beds, improving ICU patient throughput, length of stay, and costs.
Watch webinar
Healthcare Resources
Explore our healthcare resources to learn how Simul8 can benefit your organization.
Learn more
Learn more about Simul8 for healthcare process improvement
Find out more about how simulation is used by healthcare organizations, read more case studies and access a range of learning resources.
Learn more